Female Sterilization
What Is Female Sterilization?
Read More
Sterilization is a form of birth control that is permanent or should at least be considered permanent. It is an option for individuals who want to avoid becoming pregnant in the future and it’s generally very safe for most people.
How Does It Work?
Read More
Ovulation occurs every month; an egg is released by an ovary and travels down the fallopian tube for a few days. If it is fertilized by a sperm, the egg then implants in the uterus. Sterilization either blocks or removes the fallopian tubes entirely, preventing sperm from ever reaching the egg and causing a pregnancy.
Method 1: Tubal Ligation
Read More
A tubal ligation, also known as “getting your tubes tied” is the most common form of female sterilization. Conveniently, it can be performed as a postpartum (after childbirth) procedure without lengthening a hospital stay. If done postpartum, the procedure is called a minilaparotomy. After administering either general or regional anesthesia, it is done by making a small incision in the abdomen and removing a section of each fallopian tube, ensuring a complete cut of the tube.
Alternatively, a tubal ligation can be performed laparoscopically, at a time other than after childbirth. In this case general anesthesia is required, and a small incision is made in the abdomen through which a thin camera-like device is inserted and used to view the fallopian tubes. The tubes are sealed with the use of either heat or, less commonly, clips. Advantages to a laparoscopy over a minilaparotomy include a smaller incision, a slightly shorter recovery period, and a lesser need for pain medication.
Method 2: Bilateral Salpingectomy
Read More
With a bilateral salpingectomy, the fallopian tubes are removed entirely. After anesthesia is given, the procedure is performed by making 3-4 small incisions in the abdomen and removing both tubes.
Method 3: Hysterectomy
Read More
A hysterectomy is the removal of one’s uterus. This does not include the cervix, fallopian tubes, ovaries, or part of the vagina. Hysterectomies are the second most common surgery performed following c-sections.
Are there various types of hysterectomies?
Read More
Yes, there are several types of hysterectomies available. The one you receive will depend on the reason behind your need or desire for the procedure.
Hysterectomy or a supracervical or subtotal hysterectomy removes the uterus, keeping the cervix in place.
A total hysterectomy removes the whole uterus and cervix.
A radical hysterectomy removes the whole uterus, tissue on the sides of the uterus, the cervix, and the top part of the vagina. Radical hysterectomy is generally only done when cancer is present.
A hysterectomy and bilateral salpingectomy-oophorectomy removes the uterus, fallopian tubes, and ovaries.
Reasons For Getting A Hysterectomy
Read More
There are many reasons why someone would choose or require a hysterectomy; these reasons can be either elective, medically necessary, or life-saving.
Reasons include:
Sterilization
Uterine fibroids
Uterine prolapse
Cancer
Endometriosis
Abnormal vaginal bleeding
Chronic pelvic pain
Adenomyosis (thickening of the uterus)
Eliminate menstrual cycle
Affirm gender
Types of Surgical Techniques
Read More
There are two types of surgical techniques available for hysterectomies. The type of techniques performed will depend on the surgeon’s experience, reason for the hysterectomy, the patient’s location, and the patient’s overall health. The technique used will determine recovery time, risk, and level of scarring.
Open Surgery:
This is the most common approach and is typically done by going through the abdomen. The surgeon makes a 5-7 inch incision either up-and-down or side-to-side across the belly. The surgeon then removes the uterus through the incision. This method does leave a visible scar, requires 4-6 weeks for recovery, a 2-3 day hospital stay post surgery, and is at a higher price point than minimally invasive procedures.
Minimally Invasive Procedures:
MIPs allow for a faster recovery time of 3-4 weeks, less scarring and pain, lower chance of infection, and considerably lower cost than open surgery. MIPs are far superior to traditional open surgery. While we encourage everyone to do what they feel is best for themselves, we would recommend finding a physician who is capable of performing a minimally invasive procedure. There are four types of MIPs performed.
MIPS Performed:
Vaginal hysterectomy involves the surgeon making a cut in the vagina and removing the uterus through this incision. The incision is closed, leaving no visible scar.
Laparoscopic hysterectomy is done using a laparoscope, which is a tube with a lighted camera, and surgical tools inserted through several small cuts made in the belly or, in the case of a single site laparoscopic procedure, one small cut made in the belly button. The surgeon performs the hysterectomy from outside the body, viewing the operation on a video screen.
Laparoscopic-assisted vaginal hysterectomy involves the surgeon using laparoscopic tools in the belly to assist in the removal of the uterus through an incision in the vagina.
Robot-assisted laparoscopic hysterectomy is similar to a laparoscopic hysterectomy, but the surgeon controls a sophisticated robotic system of surgical tools from outside the body. Advanced technology allows the surgeon to use natural wrist movements and view the hysterectomy on a three-dimensional screen. This is the most expensive of all approaches, including open surgery.
Not everyone will be a guaranteed candidate for an MIP, please speak with your physician to discuss which procedure is best suited for you.
What to expect after your hysterectomy:
Read More
It’s important to always follow post-op procedures to ensure proper healing. Depending on the type of surgical technique used, you will spend 1-3 days in the hospital and 3-6 weeks recovering. You will not be able to lift things over 15 pounds. It’s best to take 1-2 weeks off from work after surgery, and to not have penetrative sex for 4-6 weeks. Some people will feel an overwhelming sense of relief following their recovery as they will have been liberated of their physical, mental or emotional pain, or the burden of procreation.
Benefits vs Risks
Read More
Most people are able to go home the same day as the procedure when it is performed separately from childbirth. Sterilization is effective immediately and is so effective that fewer than 1% of the patients get pregnant afterwards. It’s a positive health investment given that one won’t need to rely on hormones or any other forms of birth control anymore. While all procedures should be considered permanent, a tubal ligation can potentially be reversed. Major surgery is involved, which is not always successful, and is rarely covered by insurance.
As with all surgeries, there is a risk of infection, bleeding, or anesthesia-related complications. An additional risk of injury to other organs due to the instruments used is present for sterilization procedures. Risk of complications is increased for people with certain health conditions. The most commonly reported effects after the procedure are discomfort at the incision site and menstrual-type cramping. These can typically be managed with over-the-counter pain relievers. Effects can also include sore throat, voice loss, bloating from gas, not being able to lift for 3-4 days, and the need to sleep on one’s back.
Hysterectomy risks include excessive bleeding or clots, reactions to anesthesia, wound infection, vaginal prolapse, and fistula.
If pregnancy does occur after a tubal ligation or bilateral salpingectomy, the pregnancy is more likely to be ectopic (occurring outside of the uterus).
Regret is always a risk in life, though the majority of people are happy with their decision to be sterilized. The strongest risk factor for regret is being younger than 30 at the time of the procedure. In one study, 20.3% of women under 30 were found to regret a sterilization procedure, while that dropped to a mere 5.9% for women over 30. Further, it’s been shown that the women who express regret are typically those who misunderstood the procedure, were coerced into it, or chose the procedure due to lack of access to other birth control methods, rather than a desire to not have (or not have any more) children.
Cost
Read More
Depending on your insurance and the type of procedure, sterilization with included follow-up visits can cost up to or over $10,000. There’s a good chance that you can get the procedure at no cost or for no more than a few hundred dollars if you have health insurance, as most plans are required to cover methods of birth control, including certain female sterilization procedures. Even if there is a cost to you, it’s typically a worthwhile investment as in the long run it ends up being less expensive than paying for years of birth control.
Hysterectomies are generally covered by health insurance providers. Your OBGYN should able to contact your insurance provider to determine coverage and any costs you will incur such as your deductible. You can also reach out to your insurance provider yourself to find out which costs and fees they will and will not cover. Hysterectomies can cost anywhere from $9,000 to upwards of $13,000 out-of-pocket.
Barriers to access
Read More
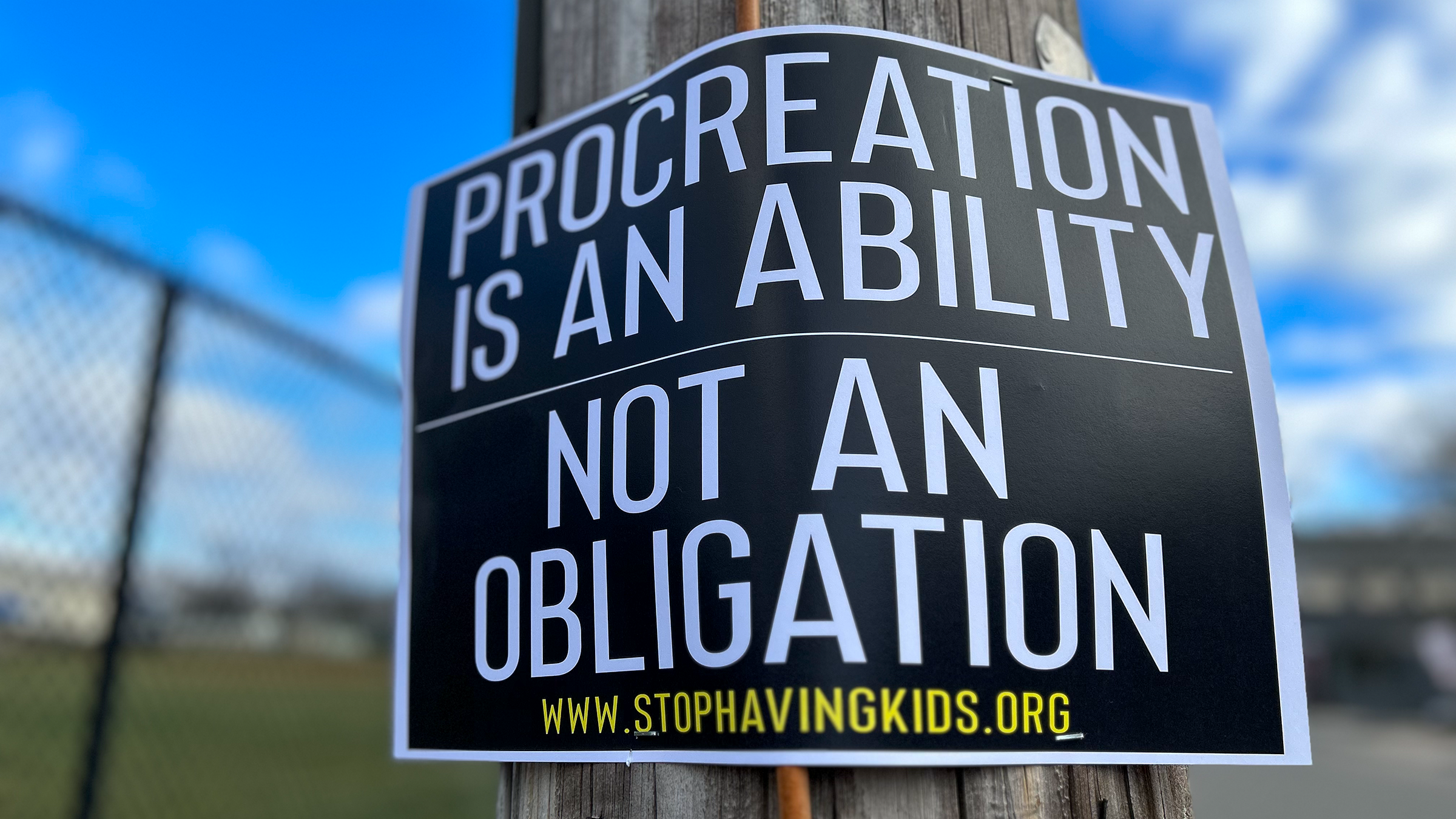
Those living in North American and some other countries who haven’t birthed any children can face many barriers to obtaining sterilization, which are rooted in sexism, religious dogma, and reproductive norms since sterilization grants females reproductive autonomy. A popular belief exists that all women want to have children and that it is a biological imperative to them. A doctor asking for permission from a husband or denying the procedure entirely due to potential future regret are not uncommon. This same concern about regret does not typically exist as much for men seeking vasectomies or women seeking fertility treatment.
To complicate things further, a history of involuntary sterilization of low-income women and non-white women exists in the US. Studies have suggested that even today’s physicians attitudes about and willingness to perform sterilization are affected by patient race, ethnicity, and socioeconomic status. Furthermore, low-income women that use government insurance often have waiting periods and/or complicated consent forms to submit before they are granted a sterilization procedure. Incarcerated women have reportedly faced pressure to undergo sterilization, while religiously-affiliated hospitals may deny the procedure. Because 1 in 6 women in the US currently receives care from a religiously-affiliated institution, this is a significant barrier.
Ethical sterilization should be focused on reproductive autonomy. It requires access to sterilization procedures for women who request them while simultaneously protecting marginalized individuals from unjust or coercive practices.
Tubal Ligation & Hysterectomy Myths:
Tubal Ligations are irreversible.
Tubal ligations procedures are usually done by either clipping or banding the tubes to block the egg from reaching your uterus, by cutting them and stitching them closed, or cauterizing them. The procedure should be considered permanent especially if your tubes have been cauterized. If your tubes have been clipped or cut, the clips can be removed and fallopian tubes reattached to the uterus or to each other but the chance of pregnancy is between 40%-85% and reversal surgery is not covered by insurance. The doctor may also deem reversal impossible if there is not enough healthy Fallopian tube left or there is no possibility to reattach the tubes to the uterus or each other, or there is too much scar tissue.
If you’ve had bilateral salpingectomy, which is the complete removal of both fallopian tubes, the procedure is not reversible.
You can still get pregnant.
Fewer than 1 in 100 females will get pregnant within a year of pregnancy and one-third of pregnancies are ectopic. An ectopic pregnancy is when a fertilized egg implants in the fallopian tubes. The more damaged your fallopian tubes, the less likely you will get pregnant.
Pregnancy after a bilateral salpingectomy procedure is so rare that there have only been 3 known cases where pregnancy occurred when both fallopian tubes have been completely removed. According to the American College of Obstetricians and Gynecologists, the rate of pregnancy for women who have partial removal of their fallopian tubes is about 7.5 per 1,000. A 2007 article published in the Singapore Medical Journal theorized that in some women who have both tubes removed the area where the fallopian tube previously connected to the uterus may not completely close over. In very rare cases, an egg might travel through the space between the ovary and the uterus and reach that opening just at the right moment. Bilateral salpingectomy should be considered nearly 100% effective at preventing pregnancy.
Your menstrual cycle will be affected.
Your menstrual cycle will not be affected as a result of a tubal ligation or bilateral salpingectomy. The only way to stop your cycle by way of sterilization is to have a hysterectomy and removing your uterus.
Hysterectomies cause early menopause.
It is rare to go into early menopause as a result of a hysterectomy. There have been some studies which show some correlation between hysterectomy and menopause. However, those studies have limitations and do not prove causation. Someone can go into surgical menopause if they have their ovaries removed. It’s important to understand that as long as the ovaries, which produce hormones, are intact it is uncommon to experience early menopause.
Hysterectomies decrease libido and orgasms.
There isn’t strong evidence that hysterectomies affect libido or orgasms. If anything, people who no longer experience pain or fear pregnancy will likely find sex much more enjoyable and pleasurable.
Hysterectomies cause incontinence.
There isn’t any strong data to support this. If you experience incontinence after your hysterectomy it could be to due complications from your surgery such as a fistula or damage done to your organs.
Hysterectomies cause weight gain.
The only weight gain one might experience is during the 3-6 week recovery period where mobility is limited. Otherwise, there is no evidence that a hysterectomy will cause weight gain. Allow yourself to heal.
Hysterectomies speed up the aging process.
This is not true. There is no evidence that hysterectomies make you age faster.
If you are experiencing trouble with finding a physician who will give you the elective sterilization procedure you'd like please see our Tips For Talking To Your Doctor About Female Sterilization page, which provides resources, information, help, and encouragement.
Sources:
https://www.acog.org/womens-health/faqs/sterilization-for-women-and-men
https://www.plannedparenthood.org/learn/birth-control/sterilization
https://www.uptodate.com/contents/permanent-birth-control-for-women-beyond-the-basics
https://pubmed.ncbi.nlm.nih.gov/10362150/
https://theconversation.com/sexist-barriers-block-womens-choice-to-be-sterilized-99754
https://www.kernodle.com/obgyn_blog/benefits-of-minimally-invasive-surgery/
https://pubmed.ncbi.nlm.nih.gov/23969830/
https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/aogs.12214
https://help.amino.com/hc/en-us/articles/360009875933-How-much-does-a-hysterectomy-cost-
https://spendonhealth.com/hysterectomy-cost/
https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/hysterectomy
https://rightasrain.uwmedicine.org/well/health/hysterectomy-surgery-myths
https://www.chicagotribune.com/lifestyles/health/sc-hlth-pregnant-no-fallopian-tubes-0612-story.html
https://www.webmd.com/infertility-and-reproduction/guide/tubal-ligation-reversal
https://www.ippf.org/blogs/myths-and-facts-about-female-sterilization